Risk Management
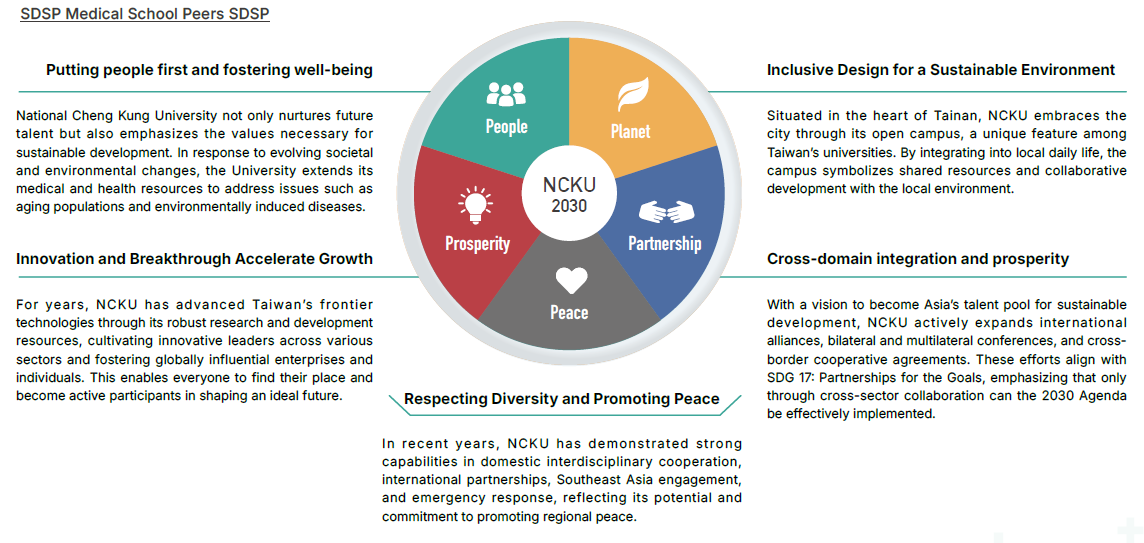
Building Sustainability Together ,Partnership Between the Hospital and the University
NCKU Hospital continues to promote sustainable operational management in line with National Cheng Kung University’s five major SDSP objectives, aiming to build a green, mutually beneficial, and thriving ecological value chain.
-
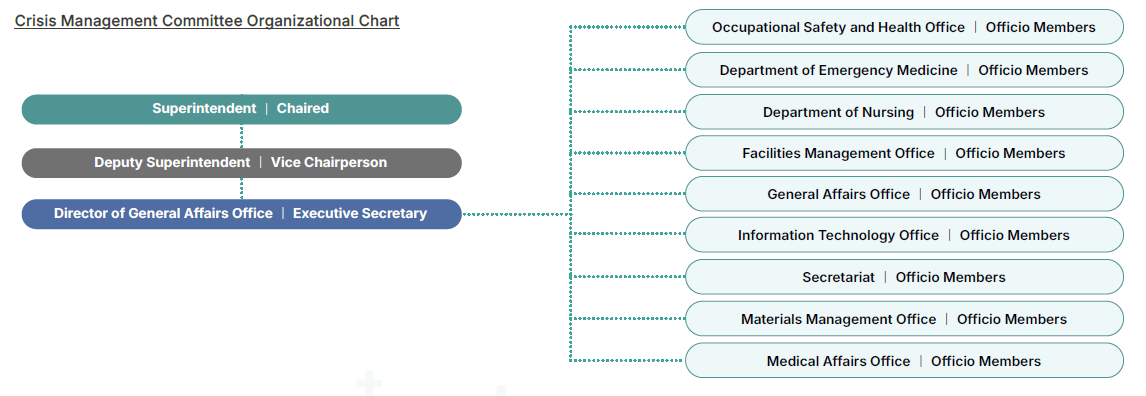
Crisis Management Committee
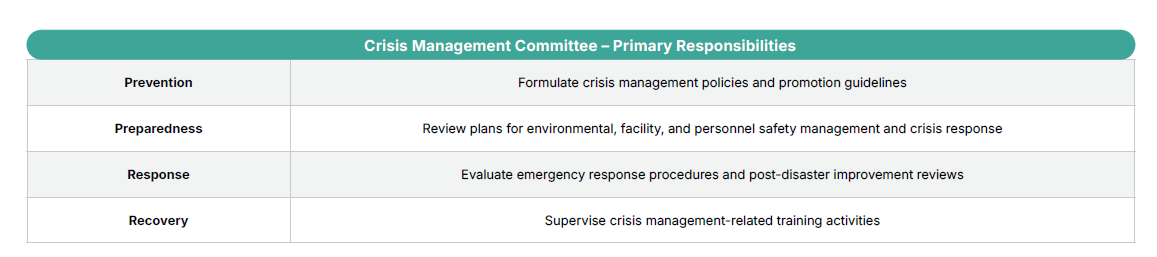
In response to the high-risk and high-responsibility nature of its national-level healthcare mission, the Hospital has established a comprehensive risk management system and formed the “Crisis Management Committee” to oversee crisis response and safety management. This committee enhances the Hospital’s organizational risk control capabilities through hazard identification, tiered response planning, and cross-departmental coordination, ensuring swift and effective handling of various challenges while maintaining the quality of medical services and public health safety.
The Committee is chaired by the Superintendent, with a Deputy Superintendent appointed as the vice chairperson. Members include heads of departments such as the Occupational Safety and Health Office, Department of Emergency Medicine, Nursing Department, Maintenance Department, General Affairs Office, Information Technology Office, Secretariat, Material Supply Department, and Medical Affairs Office, who serve as ex officio members. The Director of the General Affairs Office serves as the Executive Secretary, and other members are appointed by the Hospital Director from relevant units, totaling 19 to 21 members. Each term lasts two years, with regular meetings held quarterly and ad hoc meetings convened as necessary. All related plans are submitted to the competent authority for reference to ensure timeliness and effectiveness in emergency response and disaster management.
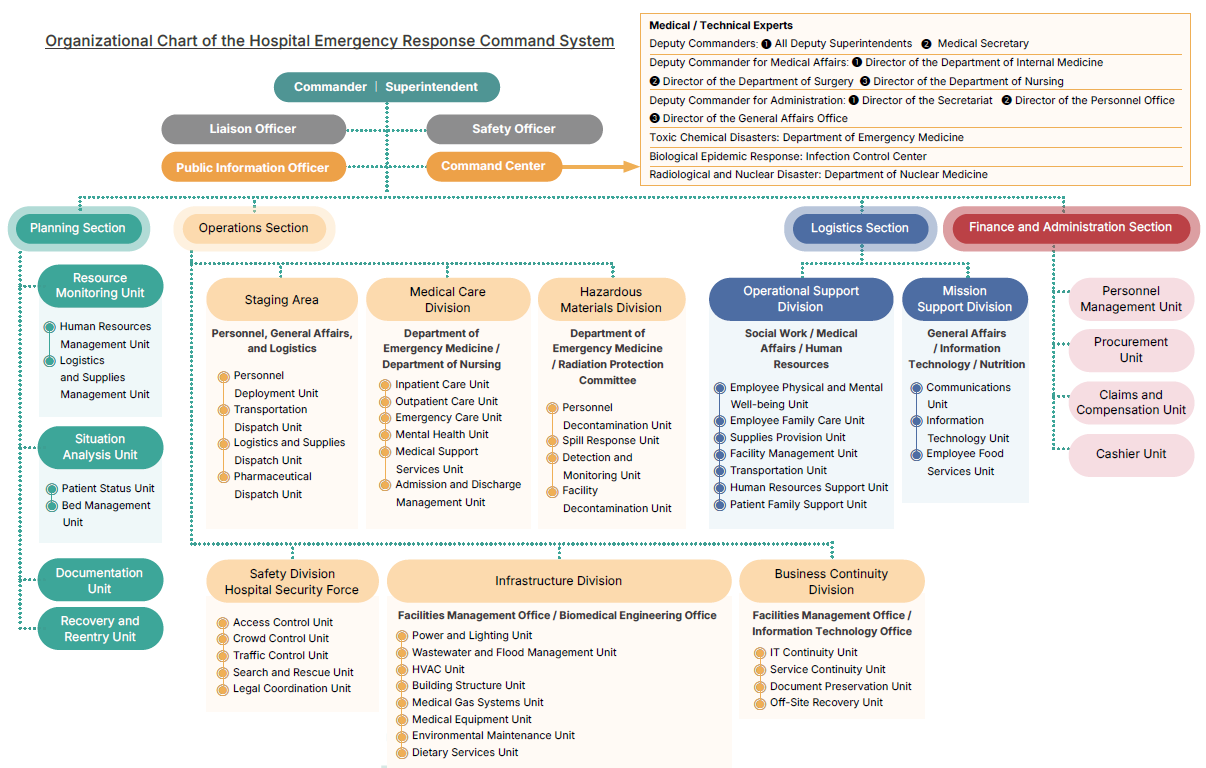
The Hospital’s disaster response system includes designated liaison officers, safety officers, and public information officers to assist with communication and information dissemination. The overall response system is structured into five main sections: Command Center, Planning Section, Operations Section, Logistics Section, and Finance/Administration Section, forming a clear vertical and horizontal communication mechanism.
The Command Center comprises a Deputy Commander and several functional commanders (e.g., medical, support, logistics) responsible for coordinating resources and operations across all sections. The Planning Section oversees resource integration and pre-disaster planning, covering manpower, material dispatch, bed management, and recovery planning to ensure the feasibility and continuity of the response. The Operations Section is responsible for frontline medical services and on-site responses, including clinical care, emergency treatment, security, traffic control, environmental inspection, and alternate site management—making it the primary executor of disaster response tasks. The Logistics Section provides comprehensive support services, such as social work, manpower assistance, material transportation, facility management, and daily necessities (e.g., catering, cleaning), to ensure the basic needs of personnel and patients are met during emergencies. The Finance/Administration Section handles human resources, procurement, accounting, and damage compensation matters, offering stable financial and administrative backing to enhance the sustainability of the entire response system.
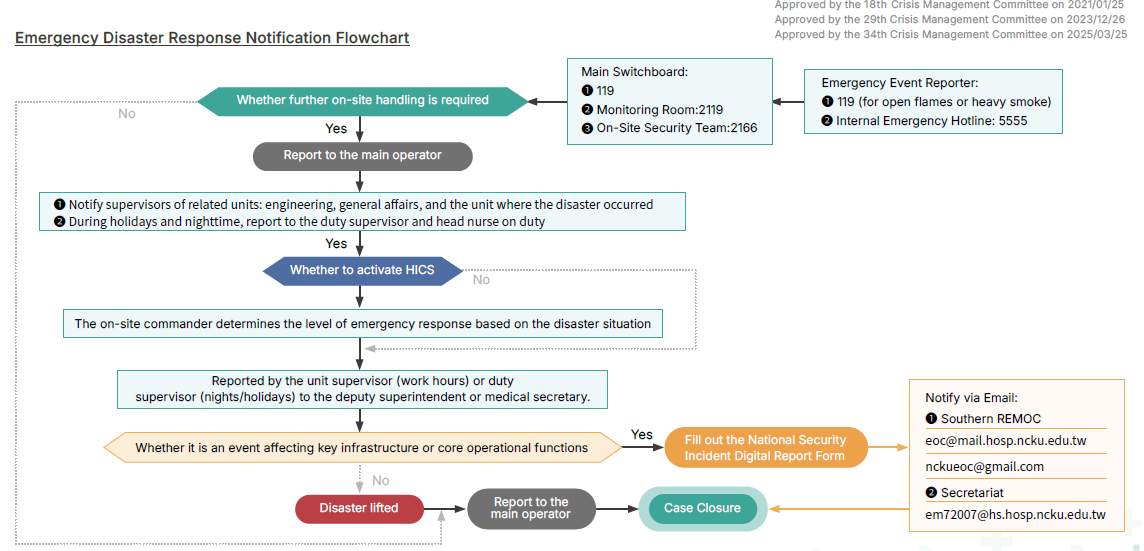
In the event of a disaster, support will be requested according to the “Emergency Disaster Response Notification Flowchart,” with a three-tier mobilization mechanism established based on the severity of the disaster to ensure the timely and effective deployment of human resources. In addition, all personnel shall carry out their assigned duties in accordance with the “Hospital Incident Command System (HICS),” forming a well-organized and orderly command chain. If the disaster results in damage to the hospital building or an influx of mass casualties from the community causes a shortage of medical resources, patients will be relocated based on the “Patient Reassignment Response Principles,” with priority given to transferring them to other appropriate sites or partner medical institutions to ensure the continuity of medical care and patient safety. At the same time, if another hospital requires evacuation support due to a disaster, the Hospital will also receive patients according to the “Patient Admission Principles,” continuing their original medical care plans and providing prompt, seamless medical support, demonstrating the Hospital’s comprehensive response capacity and commitment as a regional emergency responsibility hospital.
NCKU Hospital has established a comprehensive system for notification, evacuation, patient reassignment, and hospital isolation operations. Standard operating procedures have been developed for different types of disasters, complemented by regular tabletop drills and hospital-wide compound live exercises. Through post-disaster reviews and knowledge management feedback mechanisms, the Hospital continuously enhances its overall organizational resilience and post-disaster recovery capacity, ensuring uninterrupted medical services and patient care even during major disasters.
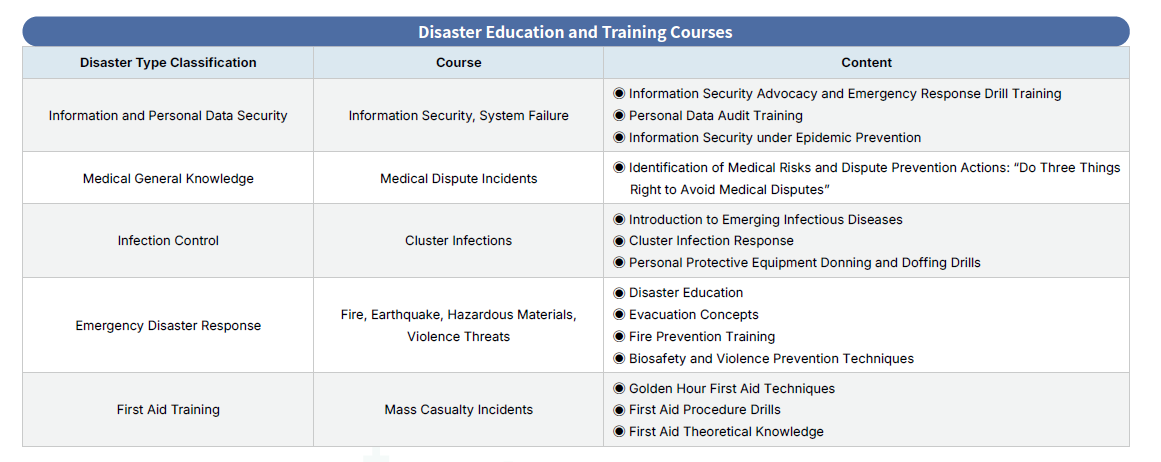
In response to increasingly diverse and unpredictable disaster scenarios, the Hospital promotes five core annual training programs categorized by disaster type, including information and personal data security, medical general knowledge, infection control, emergency disaster response, and first aid training. These programs cover areas such as cybersecurity, medical dispute prevention, cluster infection response, fire and earthquake drills, and mass casualty incident response. Quarterly drill themes are planned for high-risk periods to reinforce practical experience and frontline team proficiency.

-
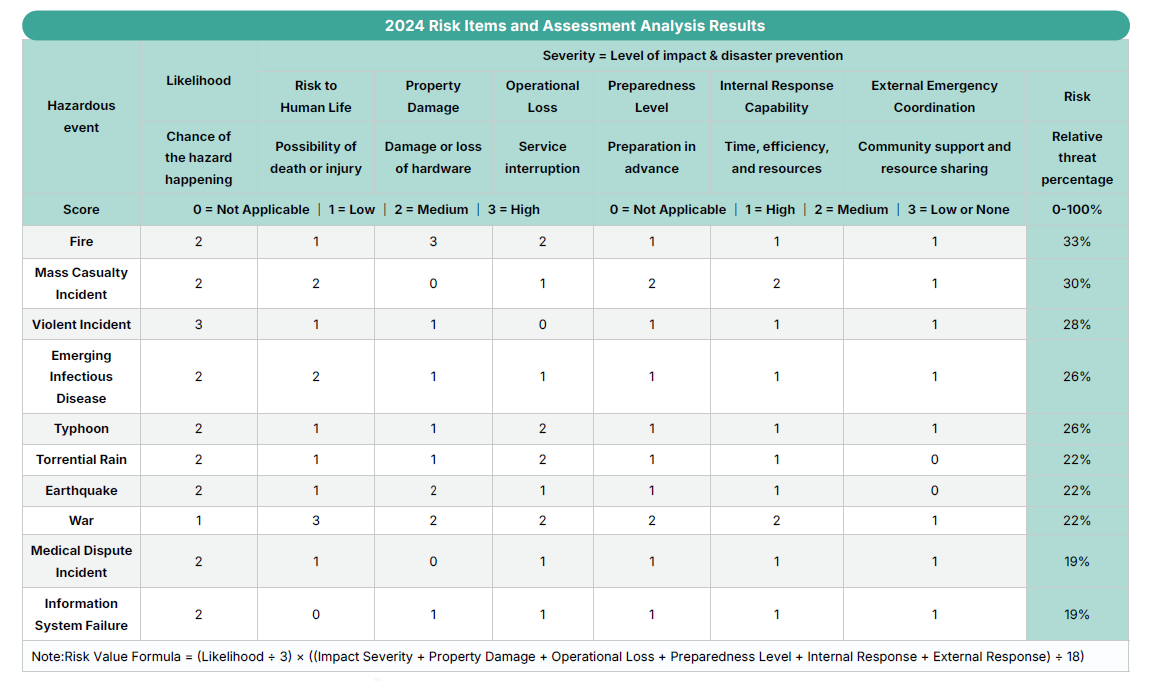
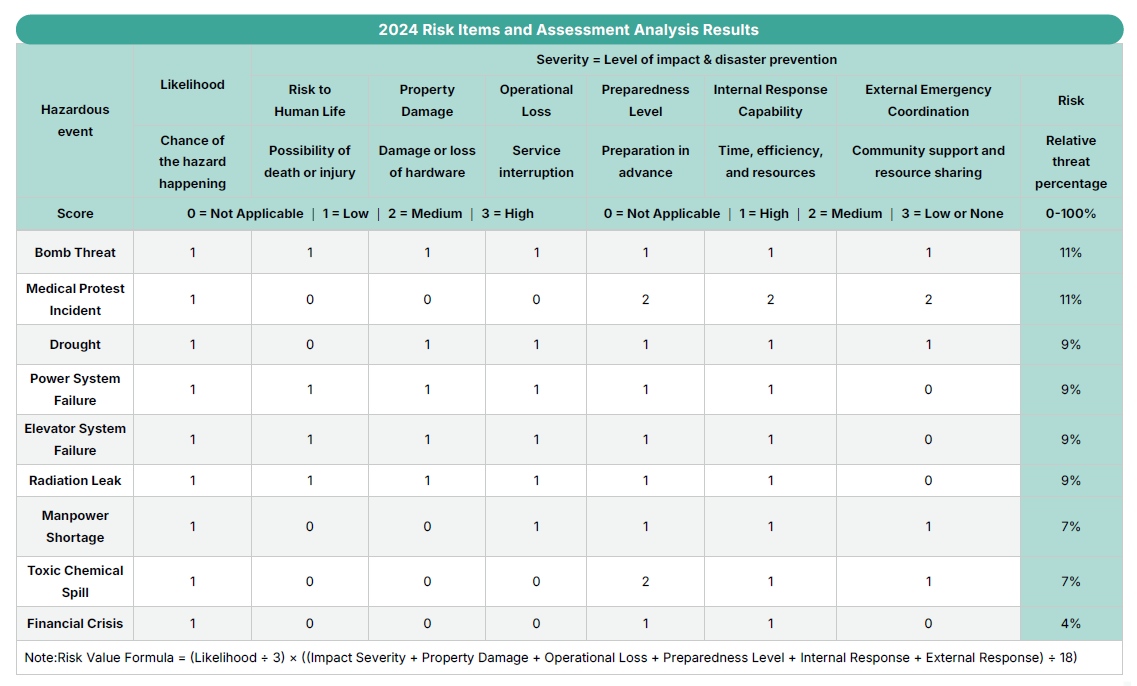
Risk Identification
To systematically identify potential threats and vulnerable areas, the Hospital has implemented the "Hazard and Vulnerability Analysis (HVA)" as a risk identification tool. Each sub-project's responsible unit forms a dedicated assessment team based on the Hospital's historical disaster experience, external environmental changes, and emerging risks—such as natural disasters and technological hazards. The team regularly inventories risk events that could disrupt medical services or threaten public safety, quantifies their likelihood and impact, and evaluates their risk values through vulnerability analysis. Risk events with a score exceeding 25% are classified as high-risk and incorporated into the Hospital’s annual crisis management priorities for ongoing monitoring. Through cross-departmental collaboration, the Hospital enhances disaster response effectiveness and the resilience of the healthcare system.
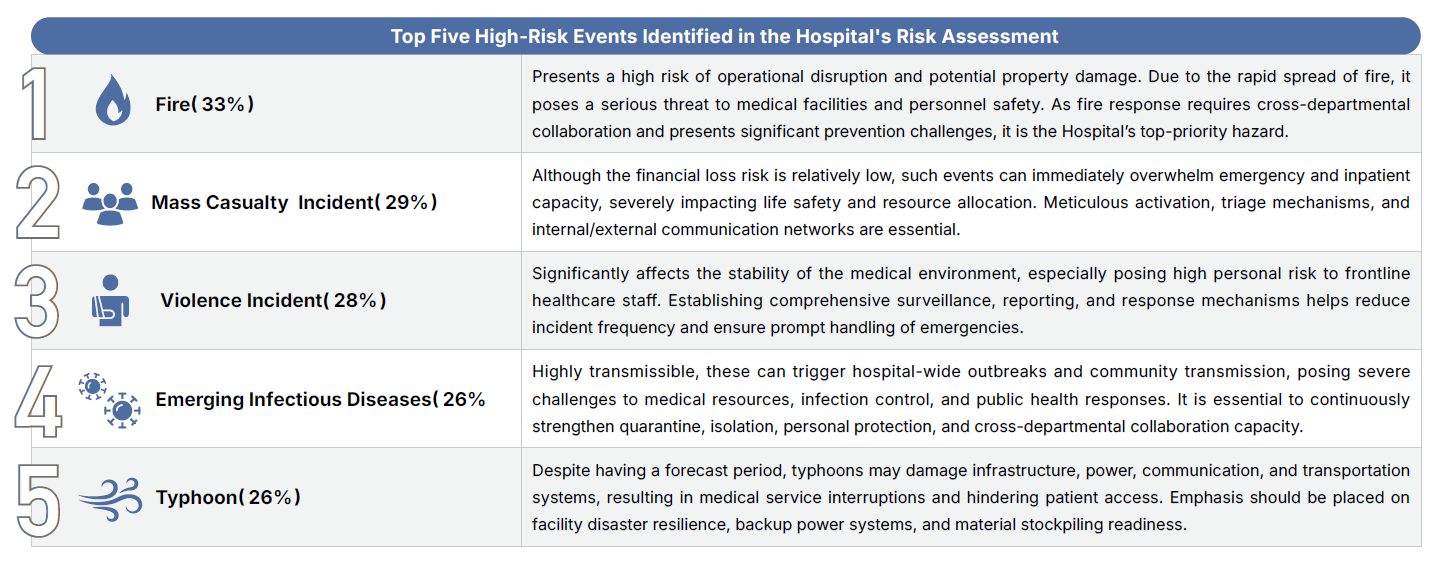
According to the Hospital’s risk assessment, the top five potential risk events are fire, mass casualty incidents, violent incidents, emerging infectious diseases, and typhoons. These events pose significant threats to patient safety and hospital operations due to their high likelihood and severe impact, and are therefore prioritized for prevention and response.
To strengthen overall emergency preparedness, the Hospital has developed specific sub-plans for each high-risk event, covering preventive measures, response procedures, command systems, manpower allocation, and post-disaster recovery mechanisms. These plans are continually refined through regular drills and training. In addition, the Hospital is actively enhancing its early warning systems, resource integration, and interdepartmental coordination to ensure uninterrupted medical services and patient safety during unexpected events.
-
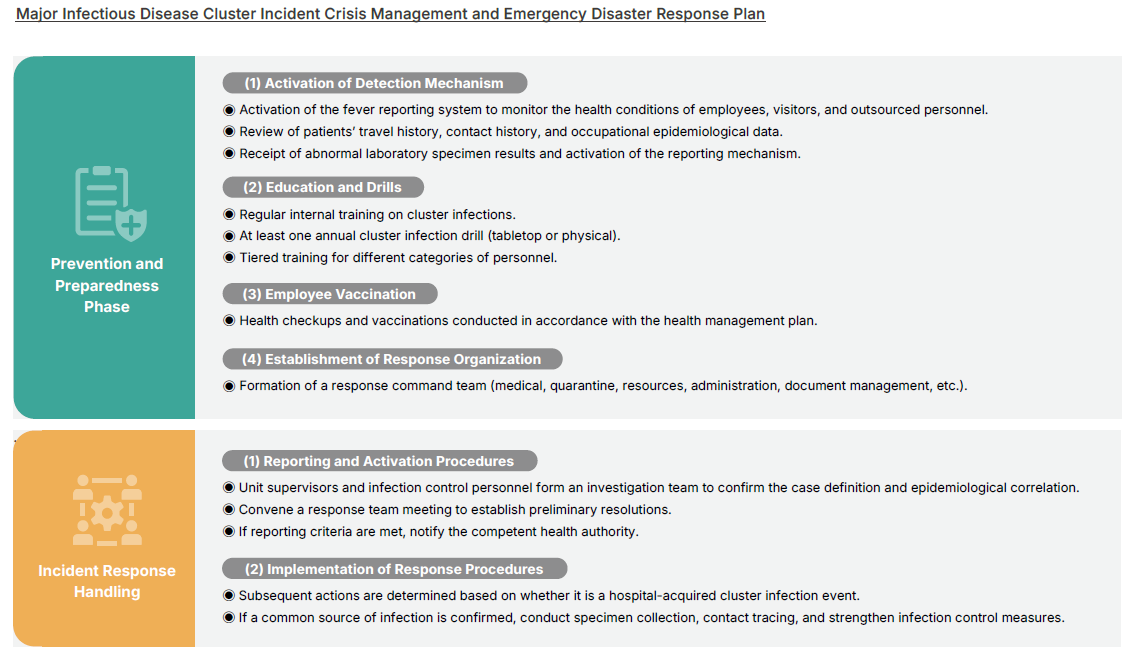
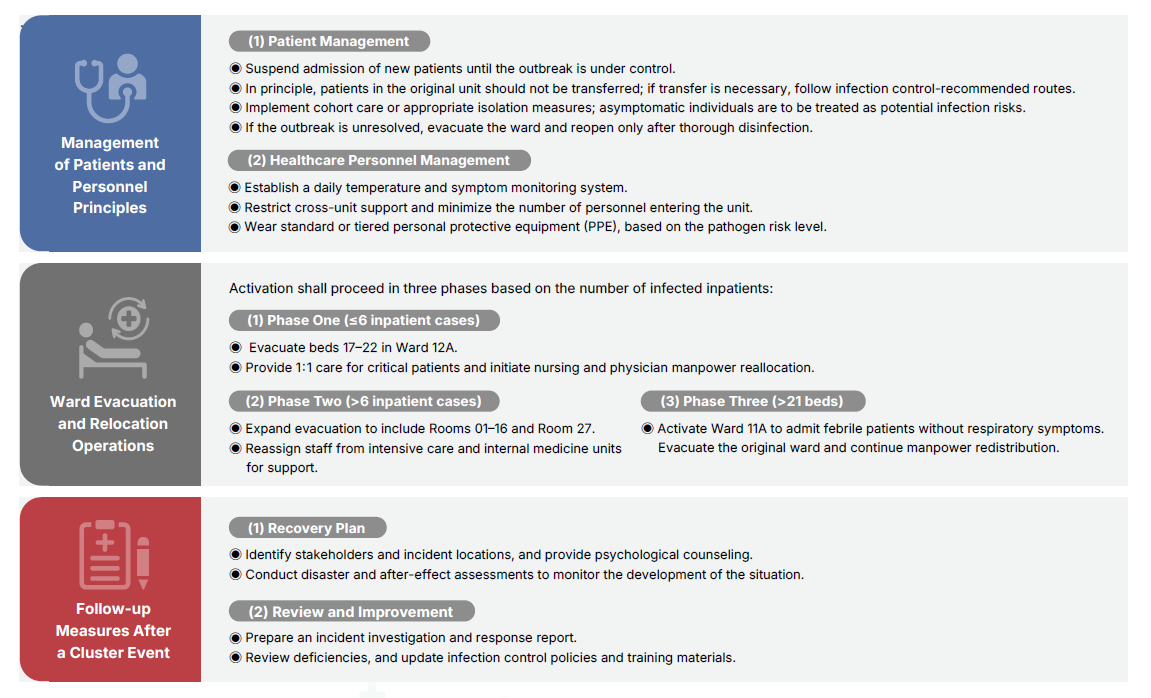
Major Infectious Disease Emergency Response Plan
The Hospital is responsible for receiving referrals and providing treatment for emergency, critical, complex, and rare diseases in the Yunlin–Chiayi–Tainan region, and also serves as a supporting hospital in the Infectious Disease Control Medical Network. To prevent cluster infections from severely impacting patient safety, healthcare workforce, and operational continuity, NCKU Hospital has established the “Major Infectious Disease Cluster Event Crisis Management and Emergency Response Plan” based on risk management principles. This plan clearly outlines reporting procedures, isolation measures, manpower mobilization, and recovery strategies. It serves as a disease prevention management guideline to be followed by all hospital staff, patients, and visitors to reduce the risk of cross-infection, ensure stable hospital operations, and maintain uninterrupted healthcare services for the community.