Responding to a Super-Aged Society
Responding to a Super-Aged Society

Wall-less Health Care
-
Integrated Geriatric Care
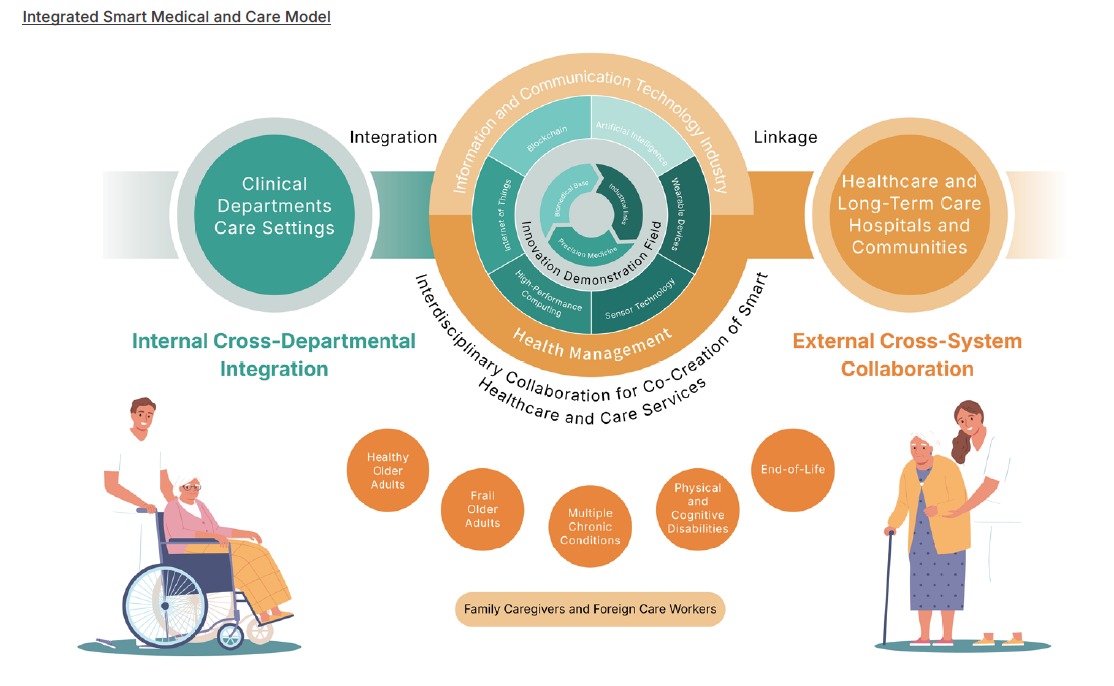
Taiwan has the fastest growing elderly population in the world and is expected to enter a super-aged society by 2025. The medical system is thus facing unprecedented challenges. NCKU Hospital is one of the few hospitals in southern Taiwan that offers specialized training in geriatric medicine. In 2019, the Department of Geriatric Medicine was established, followed by the Preparatory Office for the NCKU Geriatric Hospital in 2020. In 2022, the Department of Geriatrics was integrated into the Department of Internal Medicine. The Hospital has already integrated specialties including family medicine, rehabilitation medicine, neurology and psychiatry, nursing, physical therapy, social work, pharmacy, and nutrition to form a cross-disciplinary care team. This team promotes a “smart integrated geriatric care model centered on intrinsic capacity,” aiming to build a larger healthcare ecosystem to alleviate the burden on healthcare units and caregivers.
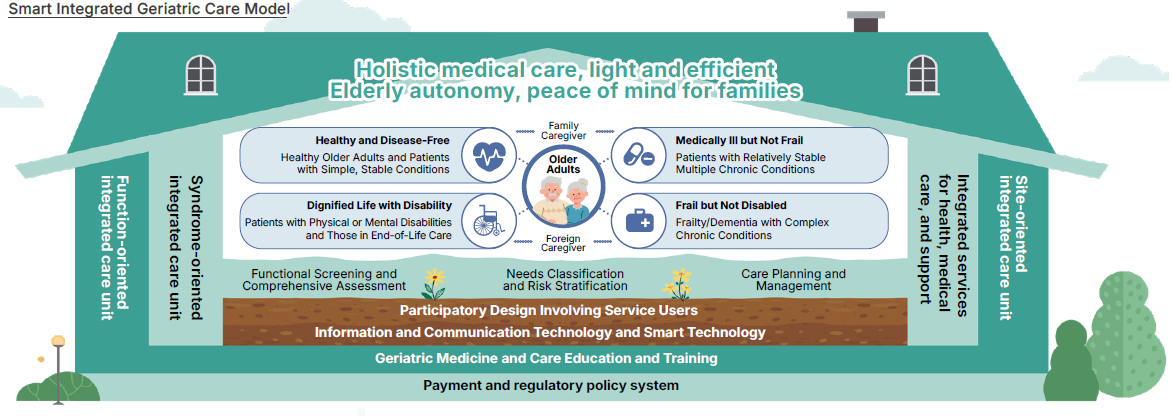
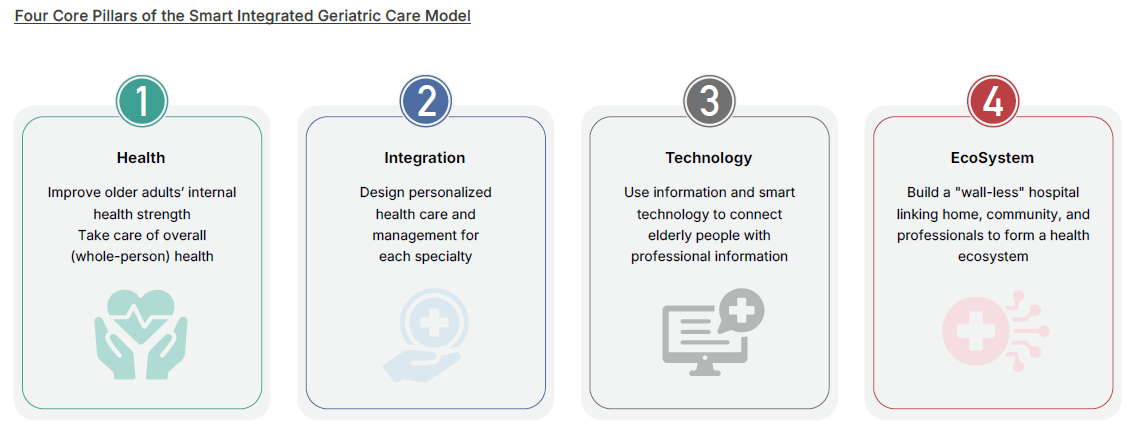
To promote transformation in contemporary health care, the Smart Integrated Geriatric Care Model is built upon four core pillars: Health, Integration, Technology, and Ecosystem. Its objective is to connect home, community, and hospital care, establishing care solutions that are functional health-oriented, syndrome-oriented, and setting-oriented, thereby addressing the diverse needs of the elderly.
“Function-Oriented” care solutions focus on the health of older adults in their daily functions, such as swallowing and chewing, nutrition, urinary function, mobility, sleep health, and cognitive and emotional well-being. These services are delivered through an integrated approach involving cross-disciplinary and cross-setting collaboration. The “Syndrome-Oriented” care unit addresses multiple chronic conditions in the elderly, including cardio-metabolic-renal syndromes, neurodegenerative disorders, and musculoskeletal diseases. The “Setting-Oriented” integrated care unit centers around various care environments—outpatient, inpatient, emergency, home, community, and long-term care institutions—by utilizing an integrated health information platform to connect home, community, and hospital-based care.
-
Taiwan’s First Geriatric Hospital
In response to national and local long-term care policies, as well as the projected massive care demands of a super-aged society, the Hospital is planning to establish a dedicated Geriatric Hospital at the Cheng Kung University Ching Yeh Campus. Serving as a hub connecting hospital, community, and home, the facility will incorporate the development and application of smart medical technologies to deliver comprehensive, dedicated care to elderly residents of Greater Tainan. This will mark the transformation of the Hospital from a traditional medical provider into an integrated platform for health promotion, disease prevention, medical care, and life support for older adults—offering an innovative model for health and care services that can serve as a valuable reference for medical institutions across Taiwan.
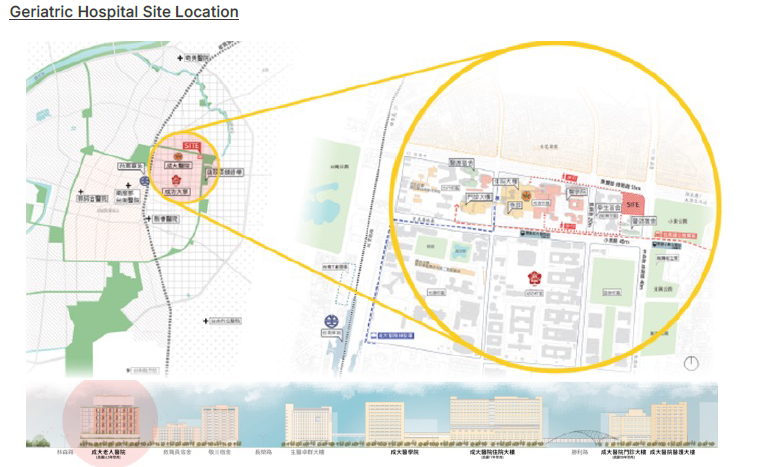
Construction of Taiwan’s first Geriatric Hospital began in 2021. The building is designed with five underground levels and twelve above-ground floors, housing approximately 450 beds to provide more comprehensive post-discharge continuous care. By integrating smart technologies, clinical data analytics, and mobile care models, the facility aims to refine the elderly care process—seamlessly transitioning patients from acute care to subacute care, rehabilitation, long-term care, and eventually home-based support.
In addition, the Hospital plans to establish an Education Center for the Development of Smart Geriatric Medical and Care Services. This center will focus on education, research, and innovation in geriatric medicine, elderly care, and smart medical technologies. It will help cultivate physicians, nurses, and caregivers well-versed in the unique medical needs of older adults, driving the transformation of the healthcare workforce toward an age-friendly structure.
-
Integration of Health Care Resources
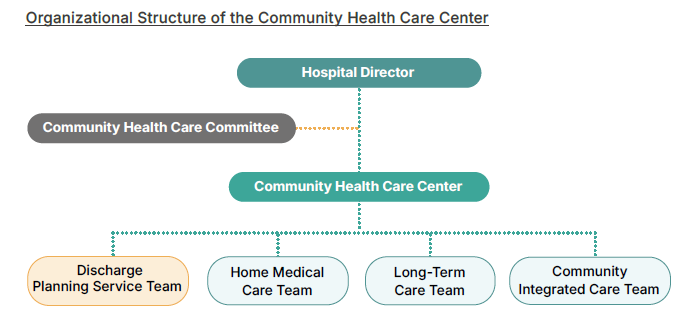
To implement the “Wall-less Hospital” policy and shift elderly care from hospitals into communities and homes—realizing a people-centered model of aging in place—NCKU Hospital established the “Community Health Care Center” in 2020. This center integrates previously independent units such as the Discharge Planning Committee, Post-Acute Care (PAC), Home Medical Care and Home Nursing Services, Long-Term Care Units A and B, Community Healthcare Groups, the Cheng-Hsing Medical Alliance, and remote area medical services into four major divisions. Cross-functional and vertical communication among these divisions has been strengthened to achieve the goal of becoming a national benchmark in community health care, thereby benefiting the public.

As Taiwan enters a super-aged society, the number of people requiring long-term care and medical services continues to rise, highlighting the growing importance of preventive medicine. In response, NCKU Hospital has made “the implementation of preventive medicine” one of its key strategies, in addition to continuously enhancing post-discharge continuity of care. By building a diverse and collaborative health promotion network, the Hospital encourages the public to shift from passive treatment to proactive health management. This aims to reduce the prevalence of chronic diseases, multiple comorbidities, disability, and dementia, ultimately lowering overall healthcare expenditures and alleviating the caregiving burden on families—thus realizing the vision of aging in place with autonomy and dignity.
In addition, the Hospital is actively promoting inter-hospital collaboration toward wall-less development. Building on the strong relationships formed with public hospitals during the COVID-19 pandemic, in 2023 the Hospital signed a memorandum of understanding with six Ministry of Health and Welfare-affiliated hospitals in the Chiayi–Tainan region. This collaboration aims to enhance the triage of mild and severe cases, leverage the strengths of hospitals at different levels, and deepen cooperation in medical care, teaching, and research, contributing to the establishment of a sound medical ecosystem in Southern Taiwan.

Healthy Aging
-
Health Assessment for the Elderly
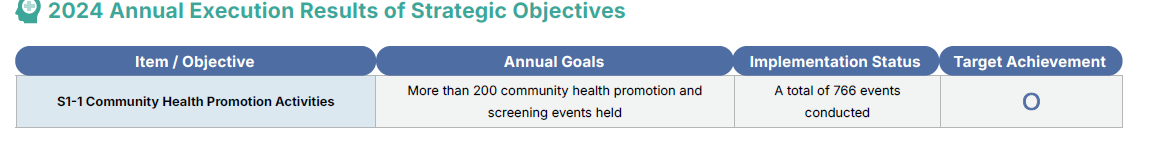
In recent years, in addition to the World Health Organization (WHO) promoting integrated care for older people (ICOPE), Health Promotion Administration has also actively advanced the “Six Functional Domains for the Elderly” screening initiative. To detect potential health issues early and prevent or delay disability, NCKU Hospital continues to conduct community health promotion campaigns. These include free screening events held during themed holiday programs, offering health promotion and lifestyle advice to encourage seniors to maintain healthy behaviors. In 2024, a total of 766 activities were organized.
In addition to promoting ICOPE, the Hospital helps older adults better understand their own health conditions. Based on each case, seniors are either referred early to the Hospital’s special clinics or provided with cooperative health management through local clinics. These efforts support the sub-healthy elderly population in maintaining good health and high quality of life.

To reduce the risks faced by elderly individuals due to oral frailty—such as sarcopenia, frailty, dementia, falls, and being bedridden—NCKU Hospital established a Chewing and Swallowing Integrated Care Team in 2020 under the Geriatric Education Division of the Preparatory Office for the Geriatric Hospital. The team is composed of more than 30 interdisciplinary professionals. In 2023, the Hospital further launched the Chewing and Swallowing Integrated Special Clinic to provide individualized diagnosis and care, and upgraded the original care team into the “Chewing and Swallowing Center.” The Center strengthens collaboration with NCKU’s Institute of Computer and Communication Engineering, Institute of Biomedical Engineering, National Health Research Institutes, and the Institute of Food Science, among other academic, governmental, and industry partners, while expanding public education activities for community members.
On the other hand, diabetes is not only one of the top ten causes of death in Taiwan, but also a major risk factor for diabetic nephropathy, cardiovascular disease, stroke, visual impairment, cognitive decline, and dementia. Therefore, the Hospital’s Diabetes Prevention and Treatment Center not only provides integrated care and continues to promote health education in the community, but also supports clinical internships and training for healthcare personnel in collaboration with relevant units. In the future, the Center will collaborate with the newly established “Dongyuan Diabetes Research Center” at NCKU College of Medicine in 2024 to promote translational medical research, integrate industry-government-academia resources, and enhance the medical care and quality of life for people with diabetes in Taiwan.
-
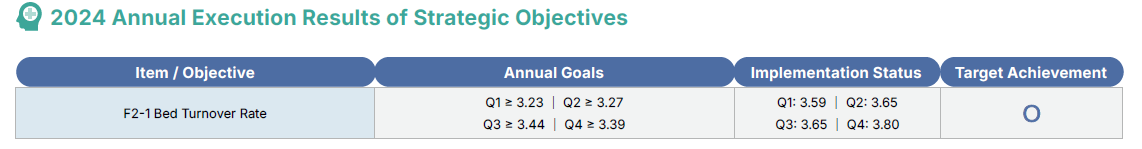
2024 Annual Execution Results of Strategic Objectives
-
Community Empowerment
“Frailty” is a geriatric syndrome that is often overlooked but has far-reaching impacts. Its symptoms include weight loss, reduced muscle strength, slower walking speed, fatigue, and decreased physical activity. Without timely intervention, frailty increases the risk of falls and disability, posing a dual challenge to family caregiving and social resources. Exercise intervention helps delay or prevent the progression of frailty into disability, reduce fall risks, and postpone entry into the long-term care system. To enable early detection and intervention for geriatric syndromes, NCKU Hospital actively collaborates with communities. In 2022, the “NCKU Ren-Ai Senior Fitness Club” was established at the Ren-Ai Community Activity Center in the Northern District, providing an age-friendly exercise venue to help the elderly maintain or improve their health through appropriate physical activity, nutrition, and social engagement.
The “NCKU Ren-Ai Senior Fitness Club” not only serves as an age-friendly exercise venue but also functions as a referral point for outpatient clinics and Long-Term Care Type A units (Community-Based Integrated Services Centers), extending the hospital’s community care services. The program is conducted in collaboration with the NCKU Department of Industrial Design, the Center for Sports Science and Healthy Aging Industry, the NCKU Hospital Departments of Social Work, Nursing, and Geriatrics. It also provides a platform for community service learning for students, community-based training and internships for staff, and volunteer opportunities for retired NCKU employees. Retired volunteers with medical backgrounds assist with blood pressure monitoring, venue maintenance, and health consultations. The exercise programs focus on integrated training such as strength, aerobic, balance, and flexibility exercises, aiming to enhance physical function and improve the quality of life of older adults. Fifteen group classes are held weekly, led by certified fitness instructors, serving an average of 300 participants per week.
In addition, NCKU Hospital has collaborated with Ren-Ai Hospital and Yi-Shiang Fitness Club for Seniors and Special Populations to establish a community-integrated health care demonstration site—“Cheng-Yi Shi-Zu.” This facility officially opened in 2024 at the former site of the Deguang Church in the Eastern District. It integrates the professional resources of the Hospital’s Long-Term Care Type A unit and leverages the multidisciplinary medical expertise of the Hospital to carry out community health promotion activities and health screening services tailored to the needs of an aging and locally rooted community, creating a localized health promotion hub.

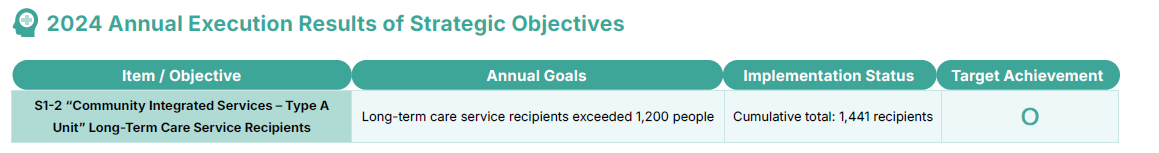
The Hospital continues to promote the integration of community health building and long-term care services. In addition to organizing community activities, visiting borough chiefs, and holding liaison meetings to educate the public on long-term care services, the Hospital also encourages community volunteers and borough chiefs to refer cases in need. This proactive approach helps monitor the health conditions of local residents, reduce the number of disability cases, and prevent delays in seeking medical care.
-
2024 Annual Execution Results of Strategic Objectives
-
Smart Technology for Health Promotion
The Hospital’s Community Health Care Center has partnered with Dynasty Clinic, a fellow member of the Tainan Diabetes Shared Care Network, to establish the “NCKUH Dynasty Smart Health Station” on the first floor of the clinic. The station features smart fitness equipment in an open space setting, embodying a spirit of public welfare and serving as a self-health promotion venue for people of all ages in the community. Officially launched at the end of 2024, the station integrates a comprehensive platform system and intelligent physical fitness devices, enabling users to instantly obtain exercise records and health reports after each session. Situated within a primary care facility, the Smart Health Station conveniently incorporates adult health checkups and preventive care services, offering accessible, community-based preventive medical services such as prevention and management of the three highs (hyperglycemia, hypertension, hyperlipidemia), diabetes care, and hypertension management.
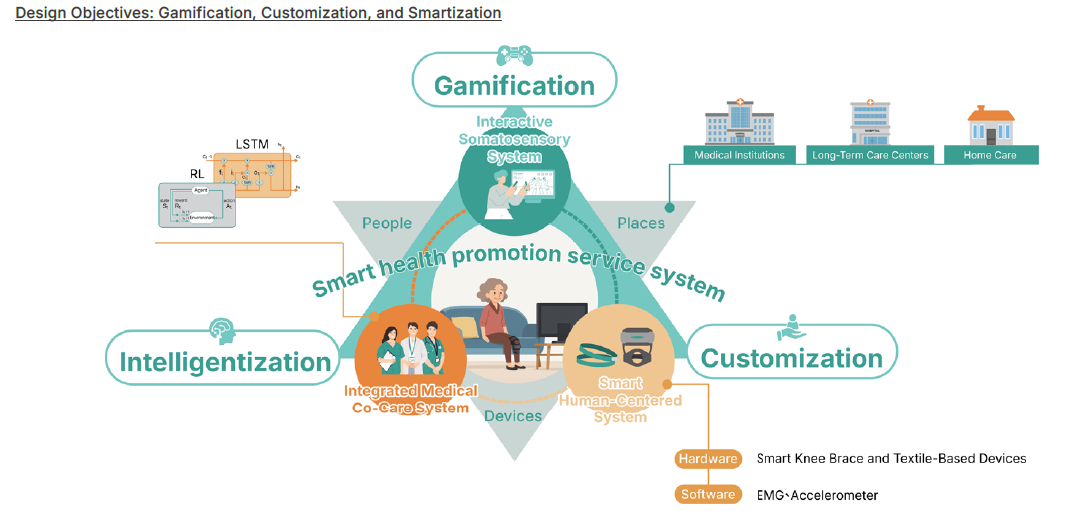
To reduce the challenges of follow-up management in health promotion and ease the care burden on healthcare providers, the Department of Physical Medicine and Rehabilitation at NCKU Hospital collaborated with aiFree Interactive Technology Co., Ltd. to develop a new intelligent rehabilitation aid—the “Smart Health Promotion Service System.”This system enables sub-healthy and functionally impaired individuals requiring muscle strength training to undergo rehabilitation at home. By incorporating nostalgic games that resonate with the elderly, it enhances their motivation for rehabilitation. During training, the system detects the condition of various muscle groups to assess the frailty level of older adults, helping professionals deliver the most accurate rehabilitation plans. Physicians can also use professional analysis reports to maintain ongoing interaction with patients and their families, thereby reducing the consumption of medical resources and improving the user’s quality of life. This service received the 2023 National Healthcare Quality Award – Outstanding Healthcare Award.
Medical Triage
-
Community Health Care
The Community Health Care Center, established by the Hospital in 2020, has the core mission of building “patient-centered holistic integrated care,” integrating “seamless care across hospital, community, home, and long-term care,” and establishing a “tiered health care network connecting medical centers, regional hospitals, and primary clinics.” As such, the original Discharge Planning Service Committee and Health Promotion Committee were merged into the “Community Health Care Committee.” Based on different core missions, four major units were established: the Discharge Planning Service Section, the Home Medical Care Section, the Long-Term Care Section, and the Integrated Community Care Section, to provide the public with the necessary health care services at various stages and to realize the principles of medical tiering and the wall-less hospital concept.
Upon admission, change in condition, or within 24 hours of transfer, an initial screening for discharge planning services is conducted by a clinical nurse to assess the patient’s current hospitalization status and potential post-discharge care needs. If the patient meets the hospital-wide or the six major medical system case acceptance criteria, a secondary screening is conducted within 72 hours. Based on individual needs, appropriate guidance and evaluation are provided. Subsequently, physicians and nurses assess the patient's physiological, psychological, social, and functional needs and, via the Hospital’s joint referral system, consult with cross-functional team members to arrange services such as disability certification, assistive device assessment, publicly funded placement, diversified rehabilitation, PAC (Post-Acute Care), or referrals to follow-up care institutions. The inter-institutional case manager for discharge planning services or the dedicated PAC case manager serves as the contact point for resource coordination.
In the past three years, 716 cases , 766 cases , and 896 cases were referred for Long-Term Care 2.0 applications, and 437 cases,402 cases and 437 cases were referred to PAC services, both showing an increasing trend. After discharge, unit nurses follow up by phone within three days to check the patient’s status and document the outcome. If the condition is stable, the case is closed; if necessary, a second follow-up call is conducted within seven days. All processes and outcomes are recorded in the medical records, ensuring the implementation of medical tiering while properly addressing patient needs.
-
2024 Annual Execution Results of Strategic Objectives
-
Post-acute Care (PAC)
There are a total of 15 hospitals cooperating with the Hospital for PAC referral, among which 6 hospitals are authorized to implement the home-based model. The Hospital has appointed four dedicated “PAC case managers” (covering stroke, fragility fractures, frail older adults, and heart failure) to serve as the liaison among the medical center, family members, and the contracted hospitals. These case managers are responsible for assessment, health education, development of interdisciplinary care plans, coordination of referrals, connection with community resources, follow-up management, and monitoring of quality indicators. In 2023, 29 cases were referred under the PAC home-based model and 3 under the day care model. In 2024, 26 cases were referred under the PAC home-based model and 19 under the day care model.
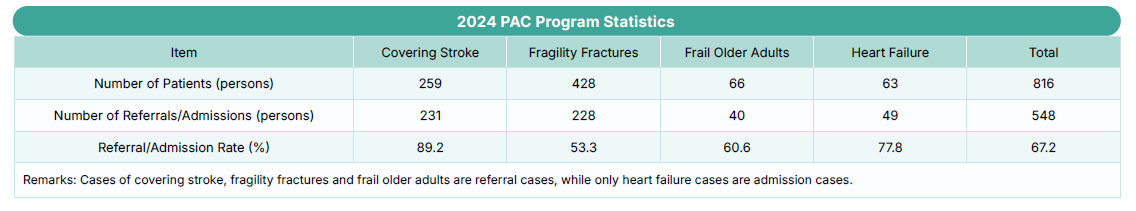
In addition to facilitating the proper allocation of medical resources, the NCKU Hospital PAC team has also continued to improve its case management capabilities and actively participated in quality indicator competitions. In 2023, the team received the Excellence Award in the “Southern Region Integrated Post-Acute Care Model Program” by the Southern Regional Healthcare Network. In 2024, the Heart Failure PAC team was further recognized with a Gold Award in the “Taiwan Healthcare Quality Award.” The Hospital also co-organized the “Post-Acute Care Training Course for Frail Older Adults” with the Tainan City Public Health Bureau to train new talent and enhance the region’s overall ability to care for PAC cases. Furthermore, the Hospital’s Stroke PAC team achieved the third-highest referral rate among all medical centers nationwide in both 2022 and 2024, demonstrating the Hospital’s active promotion of the PAC program and effective implementation of the hierarchical medical care policy.
It is worth mentioning that stroke patients must receive thrombectomy within the golden window of three hours after onset to reduce the risk of severe sequelae. With the support of a comprehensive stroke team, the Hospital ensures that patients receive the best possible treatment and care.
For details regarding emergency medical services, please refer to Section 3.3.2 “Greater Tainan Emergency Medical Services.”
-
Home Medical Care – Acute Care at Home (ACAH)
In order to enhance the integration of medical care and long-term care services and allow more elderly people to “age with support, age with care, and achieve local end-of-life care,” NCKU Hospital has established a cross-departmental team to integrate resources from nearby regional hospitals, primary care clinics, and home nursing institutions, dedicated to building a comprehensive acute care at home (ACAH) network. A telemedicine platform is adopted to strengthen the quality of acute home care services.
The promotion of home medical care and ACAH enables patients and their families to receive professional care without the hassle of traveling back and forth to the hospital. Through the use of IoT monitoring systems, vital signs and oxygen levels are tracked, allowing case managers to grasp physiological changes of patients in real time via the care platform. Home nurses conduct regular home visits for physical assessment and medication administration, while physicians assess the patient's condition daily via video consultation or home visits. This not only reduces the burden on patients and families, but also helps maintain a familiar lifestyle and improve quality of life.