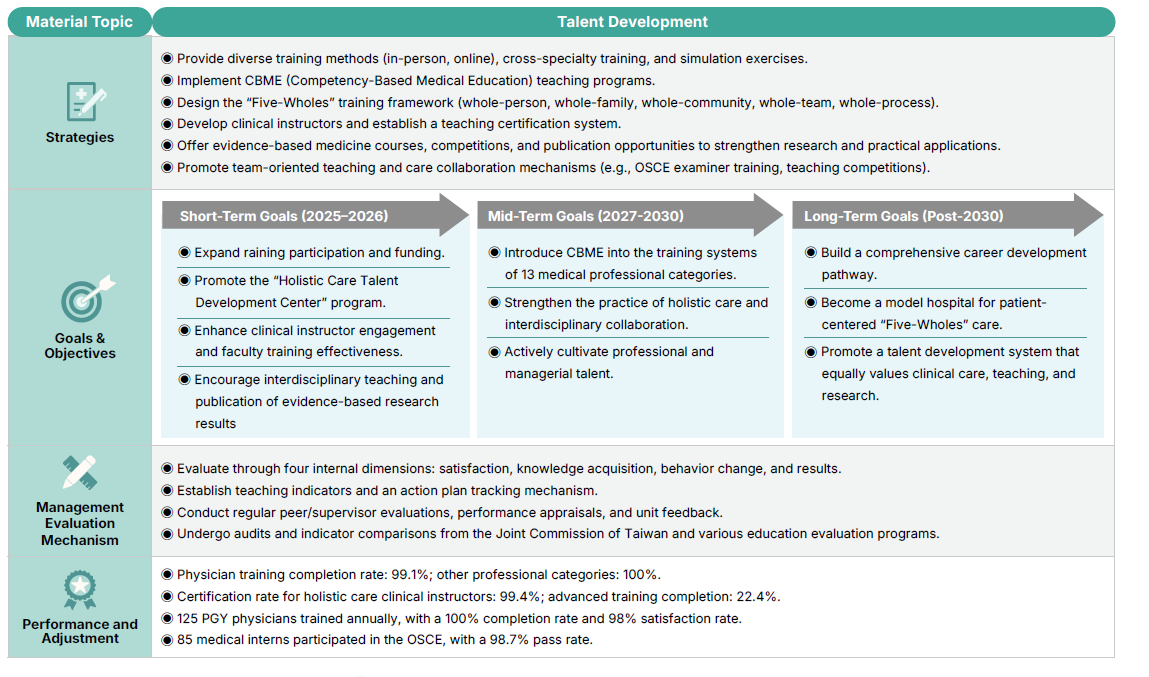
Cultivating Medical and Nursing Talents
Cultivating Medical and Nursing Talents

Shared On-campus Resources
-
Clinical Skills Center
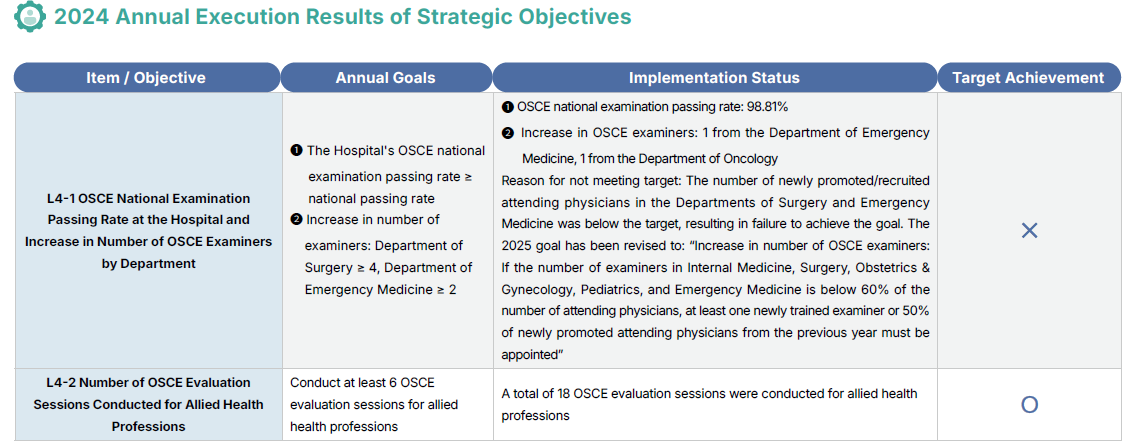
The Hospital’s teaching materials room, through the classroom management system, assists staff in reserving training space at the College of Medicine B1 “Clinical Skills Center.” This center serves as a national OSCE testing venue, capable of conducting 12-station objective structured clinical examinations (OSCE) for Western medicine physicians and healthcare personnel. It is also used for routine clinical skills practice, including clinical medical diagnostic training, nursing personnel clinical skills education, emergency team training, and skills training for UGY and PGY.
The Clinical Skills Center is equipped with fully functional simulated consultation rooms, intensive care units, and various computerized models for cardiopulmonary resuscitation, tracheal intubation, nasogastric tube insertion, and catheterization. These facilities enable medical staff to integrate basic medical knowledge with humanistic care, transforming it into clear clinical reasoning, thereby allowing them to accumulate sufficient clinical training experience before directly engaging with patients.

The OSCE examination is part of the physician national licensure qualification, jointly organized by the “Medical Clinical Skills Examination Affairs Committee” composed of teaching hospitals accredited by the Ministry of Health and Welfare, the Taiwan Medical Education Association, the Ministry of Health and Welfare, the Ministry of Education, and the Ministry of Examination of the Examination Yuan. Candidates are assessed using “standardized patients” (certified patient actors) in areas including medical history taking, physical examination, clinical judgment and patient management, communication and health education, attitude, and professional conduct, as well as demonstration of basic clinical skills. In 2024, 85 of the Hospital’s medical interns participated in the OSCE, achieving a pass rate of 98.7%. NCKU Hospital is one of the national examination venues for this test, responsible for overall examination planning and organization.
NCKUH Teaching Center
-
Internal Teaching Operation and Division of Labor
The Teaching Center is a first-tier unit of the Hospital, responsible for the coordination, planning, and implementation of all hospital-wide teaching courses and activities. Upholding the mission of being “the driver of training quality in medical centers,” the Center aligns with the Hospital’s vision and strategies, striving to enhance teaching quality and cultivate comprehensive, high-quality healthcare professionals across various fields. It also establishes partnerships with all departments throughout the Hospital, working together to fulfill the Hospital’s educational mission and realize the vision of “becoming a top-tier teaching center among domestic medical centers.”

The Director of the Center is responsible for setting objectives and overseeing the management of teaching affairs. The Executive Director integrates and supervises teaching operations, while the Deputy Director coordinates and handles various tasks within the Center. Teaching Attending Physicians plan and implement teaching-related work. Based on the nature of its missions, the Teaching Center is organized into four divisions: Faculty Development Division, Skills and Information Division, Medical Education Division, and Allied Health Education and Staff Training Division. Within the Medical Education Committee, there are ten teaching task forces: Interns, PGY, Residents, Allied Health Professionals, Clinical Skills, POMR, Interprofessional Teams, EBM, Medical Ethics, and CBME task forces. A “Staff Basic Education Training Review Meeting” is held every six months to track course implementation results and revise the annual “Staff Basic Course Education Training Plan” accordingly.
In 2024, the physician training achievement rate reached 99.1%, and other professional categories achieved 100%. A total of 125 PGY physicians completed training, with a 100% completion rate and 98% satisfaction rate.

-
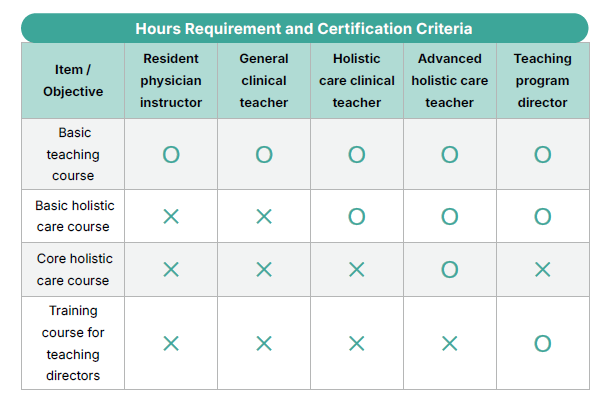
Clinical Faculty Development
NCKU Hospital encourages newly appointed attending physicians to proactively participate in the “Clinical Teacher Instructional Training Program” and actively increases the proportion of “Advanced Faculty in Holistic Care” throughout the Hospital. Hospital-level guidelines, including the “NCKU Hospital Clinical Faculty Development Guidelines” and the “NCKU Hospital Faculty Development Program,” have been established.
The Faculty Development Division of the Teaching Center designs relevant training programs based on the professional knowledge development of each discipline and clinical care needs, following the development guidelines and the Faculty Development Program (which includes holistic care). Courses cover teaching theories and regulations, teaching material creation, instructional methods and curriculum design, teaching assessment, communication and feedback, and holistic care medical education, aiming to cultivate professional talents in medical education.
In developing clinical teachers, the Teaching Center adopts the widely used “Kirkpatrick Model” from the fields of educational training and human resource development to assess whether teachers can truly internalize and transform instructional methods into daily teaching practices—for instance, adopting more systematic bedside teaching, more effective feedback strategies, or proactively guiding students to shift their clinical thinking.
This evaluation approach not only promotes continuous self-reflection and improvement among faculty but also aims to achieve the goal of “transforming teaching behavior and enhancing educational quality.”
To recognize faculty devoted to instructional training, the Hospital has established the “Guidelines for Selecting Outstanding Teaching Faculty and Excellent Teaching Units” and the “Guidelines for Teaching Innovation and Achievement Presentations.” Through public awards and bonus incentives, the Hospital aims to foster a stronger teaching culture and enhance the quality of clinical medical education, bedside teaching, and training practices. In 2024, the certification rate for holistic care clinical faculty reached 99.4%, with 22.4% completing advanced training.



